Week 2 Post-Op Bariatric Surgery Instructions
Medically Reviewed by Katelyn J. Mock, US-Registered Dietician (R.D.)
You would still have some IV fluids from the hospital. So, if you are not losing weight two weeks after bariatric surgery, stay patient. It is coming.
For gastric bypass and gastric sleeve patients, you should now be following a full liquid/pureed diet, as long as you have no major intolerance issues with the previous clear liquid stage.
Changes in Bowel Movements
You have probably noticed a change in your stool consistency and frequency in the past 7-14 days since surgery.
It is normal to have some constipation or less stool than usual and softer consistency in bowel movements as well. There are a few main causes of this change.
- First, the amount of food you are consuming is less, and as a result, you will have fewer bowel movements.
- The pain medications that you took or are potentially still taking after surgery can also frequently lead to constipation, as can calcium and iron in your vitamin regimen.
- Reduced physical activity can be another cause of constipation after surgery.
- The initial post-op liquid and pureed food diet is also significantly less fiber than you are likely used to consuming.
Nutritionist Explaining Constipation after Bariatric Surgery
What can a Bariatric Patient Take for Constipation?
- If you are experiencing hard stool that is difficult to pass, you are likely not getting enough fluids during the day.
- Increasing your fluid intake, and adding more soluble fiber-based foods to your diet can help.
- Try soft-cooked lentils that have been blended, mashed avocados, or pureed split pea or bean soup.
- Drinking warm water with lemon may also help.
- Mixing 1 Tbs. of flax oil into Greek yogurt may relieve constipation as well.
- Remember to eat 4-6 smaller liquid or pureed meals daily and to drink/eat slowly.
Your new stomach has a much smaller reservoir to store food now, and it takes some time to get used to that new feeling of fullness. A common, tolerable amount of food is a quarter or half a cup per sitting.
Some foods will make you feel full faster, and that is okay. It is also normal for foods to be well accepted one day and then cause some problems, like nausea or vomiting the next day.
Try to take the whole process in stride, it is normal for the “new” stomach to be sensitive.
Here are some tips for how to blend and pureed foods [1]“The Bariatric Diet” Wexner Medical Center, The Ohio State University
View in Article
- Start by cutting food into small pieces.
- Add a broth, milk or other liquid to the blender.
- Strain foods that are not smooth.
- Don’t be afraid to add spices and herbs for flavor.
Caring for Incisions
Infection is rare but is one of the more dangerous risks of any surgery. Follow the aftercare given for your incisions closely.
It is normal to have some drainage, but if your wound becomes reddened, swollen, yellow or greenish in color, odorous, pus producing, increasingly sore, or you experience a fever, seek medical attention immediately. – The University of California at San Francisco
Taking Vitamin and Mineral Supplements
If you haven’t already, start to add in some bariatric specific vitamins.
Many patients do best with chewable supplements at this point in time.
It is important to think of your new vitamin/mineral regimen as medication. These nutrients aid in proper body functioning and deficiency in certain nutrients can lead to serious negative side effects and can even be potentially life-threatening.
Some trusted brands include Celebrate Vitamins, Bariatric Advantage, Bariatric Fusion, ProCare Health Bariatric, Nestle Optisource. After surgery, you will want to take a Multivitamin, Calcium, Vitamin D, Vitamin B12, and Iron, if your multivitamin does not already contain iron.
Here are some guidelines by the American Society for Metabolic and Bariatric Surgery (ASMBS) for the amount of each nutrient that is recommended in your supplement. [2]“Nutritional Guidelines” American Society for Metabolic and Bariatric Surgery (ASMBS)
View in Article
Here’s a list of the required daily dosage of nutrients
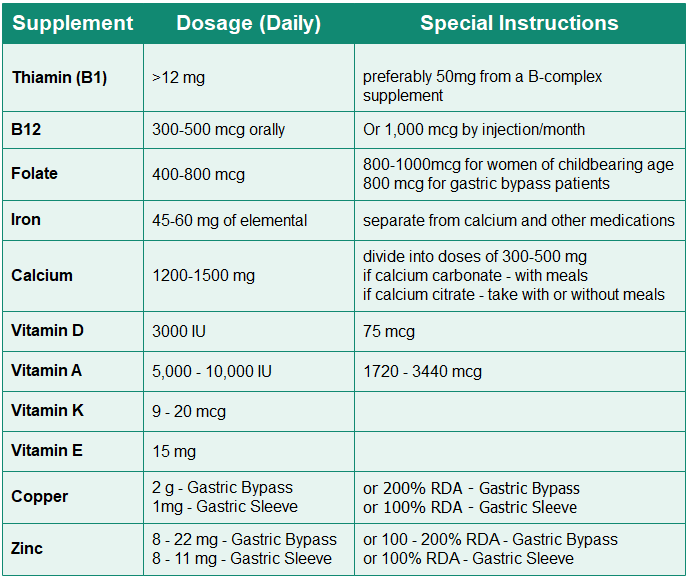
- Take your calcium separately from your iron-containing vitamin as they compete for the same absorption sites.
- For Vitamin D, D3 or Cholecalciferol is recommended over D2 or Ergocalciferol
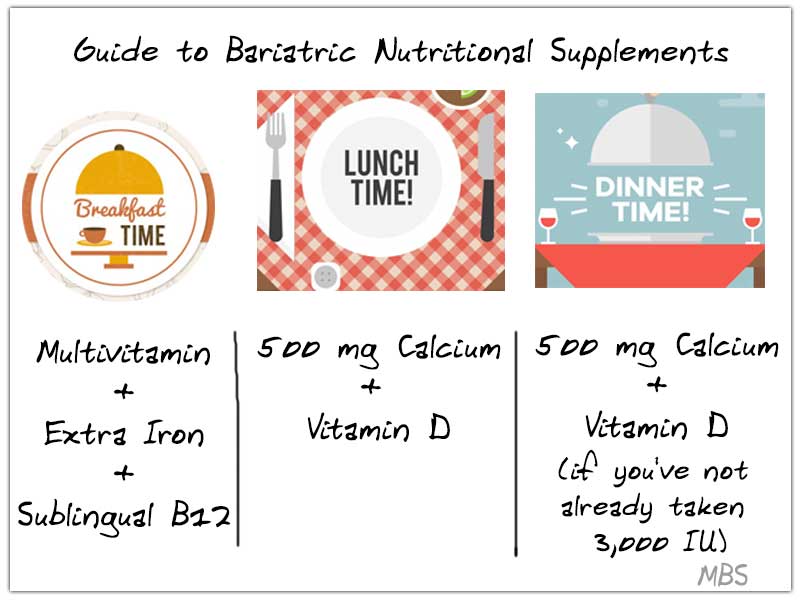
Organizing Nutritional Supplementation
Below is an example of how you can organize your vitamin/mineral regimen
Breakfast: Take Multivitamin, additional Iron, and sublingual B12.
Lunch: 500 mg of Calcium + Vitamin D.
Dinner: 500 mg Calcium + Vitamin D (if you haven’t already taken 3,000 IU).
Bedtime: 500 mg of Calcium + any remaining Vitamin D.
If you notice that you have nausea after taking the iron supplement, try having any iron-containing medications before your bedtime snack.
Tip of the week:
Watch the second hand on a clock to make sure you are not taking more than 2 bites per minute. This will seem mundane at first but will help train you to slow down at meals.
Avoid taking bites larger than the size of a dime or sips larger than 1/2 teaspoon. Keeping a dime on the table while you eat is a good reminder.
References
- “The Bariatric Diet” Wexner Medical Center, The Ohio State University
- “Nutritional Guidelines” American Society for Metabolic and Bariatric Surgery (ASMBS)


